People with diabetes are more prone to blood vessel flow problems known as peripheral vascular disease (PAD) and nerve ending issues, called neuropathy. Excess glucose creates damage to your blood vessels and nerves – especially the smaller vessels – and weakens your veins. Although there is no direct link between diabetes and varicose veins, many people suffer from these conditions simultaneously. “50% of people 50 and over have varicose veins”. Although not as troublesome as neuropathy or PAD, varicose veins can be painful and troublesome. They are more common in women due to their fluctuating hormone levels but are seen in men as well. Varicose veins can have a negative impact on blood circulation. The ugly appearance of blue, purple, thick veins up and down your legs may be of great concern, too. Let’s examine the important factors relating to varicose veins:
What are Varicose Veins?
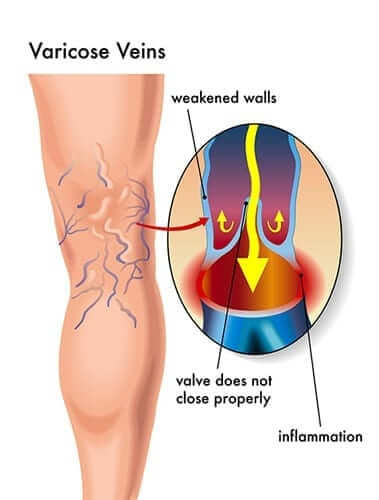
Varicose veins are enlarged, elongated, bulging blue and purple veins that resemble cords and are twisted directly under the skin due to relaxed vein walls. Your veins have a one-way valve “that prevents blood from flowing backwards due to the pull of gravity”. Over time, and for specific reasons, the vein valves become faulty and relax. Some of the blood, which should be traveling to your heart, backs up and pools in the veins. This increased pressure continues to weaken the vein walls. Besides large varicose veins, the relaxed valves can cause spider veins which are smaller, superficial and mostly cosmetic. Varicose veins usually appear on the calves or on the insides of your thighs. Varicose veins can also cause venous insufficiency, which is a true circulation problem that can occur in deeper veins and cause blood clots.
What are the Risk Factors of Varicose Veins?
- The biggest risk factors is your heredity and family history
- Being over the age of 50
- Being pregnant, which increases blood volume and hormones
- Going through menopause which causes hormone fluctuations
- People who stand most of the day such as nurses, teachers, surgeons, flight attendants, hair stylists and operating room technicians – they all experience a higher risk of varicose veins
- Obesity causes added weight and pressure on your veins
- Having chronic congenital heart valve conditions
What are the Symptoms of Varicose Veins?
- Swelling in the ankles or legs
- Tingling in the legs, fatigue in the legs
- Redness, throbbing, aching, heaviness in the legs
- Chronic inflammation, cramping, darkening of surrounding skin
- Fullness and a possible rash
- Muscle cramps
- Dry, itchy, thin skin around the vein
- The symptoms tend to be worse after long periods of sitting or standing in one position
What may happen when you have Varicose Veins?
Because of the pooling blood in your veins, you are more at risk for blood clots, infections, sores and skin ulcers in that area of the vein. Avoid sitting and standing still for long periods of time. Skin ulcers occur because of fluid buildup and pressure from the blood in your veins. People who have varicose veins can suffer from “thrombophlebitis”, which is a blood clot within the varicose vein.
Generally superficial, thrombophlebitis is more common with varicose veins. It can cause the vein to become red and hard. Treatment for the superficial kind of phlebitis is an analgesic such as aspirin and elastic support hose. If not treated, the clot could travel to the lung, which is called a pulmonary embolus. A pulmonary embolus can cause shortness of breath and become a critical medical problem if not treated. Always report any change of color, tenderness or hardness in your varicose veins to your physician.
Having varicose veins may also increase your risk of cellulitis, which can become a severe medical problem if it isn’t identified or treated. According to the Mayo Clinic, “cellulitis is a potentially serious bacterial skin infection. It appears as a swollen red area of skin that feels hot and tender”. Although they can appear anywhere, varicose veins usually appear in the lower leg area. Because diabetes can weaken your immune system, your risk for cellulitis increases – especially with varicose veins.
Cellulitis can appear as:
- Red blisters
- Open blisters
- Severe tenderness
- Skin that is hot to the touch
- Local swelling
- Inflammation
- A fever
The swelling vein may cause a break in the skin which allows streptococcus or staphylococcus bacteria to enter. If not treated, the infection can spread to the blood stream and lymph nodes developing into a life threatening condition.
How do you diagnose varicose veins?
A complete medical history (including family history), as part of a typical physical exam (including height, weight and palpation [or touching and squeezing] of your veins), helps with the diagnosis. A Doppler or Duplex ultrasound scan checks the blood flow in your legs. The Duplex ultrasound is a non-invasive test. The vascular specialist places a hand-held transducer against your skin, starting in the groin area and continuing down to your ankles. The transducer sends the image to a monitor using high frequency sound waves. The ultrasound shows instant information to the physician who can then make informed decisions on how your vein problems should be treated. These tests are pain-free and non-invasive.
Possible Natural Remedies for Varicose Veins
Here are a few natural ways to help with varicose veins. This is not a fix for an acute vein problem, such as cellulitis. Always check with your health care provider prior to trying out natural ways to treat your varicose veins. If approved, you might want to give these options a try.
Activities:
- Exercise, along with helping your diabetes, is one of the best ways to tame varicose veins, since it stimulates blood flow. Most forms of aerobic exercise work, such as walking, running, cycling, rowing, climbing up and down steps, or using an elliptical machine. One of the best forms of exercise for positive vein health is swimming laps or engagine in water aerobics. According to Dr. Jon Matsumura, chair of vascular surgery at The University of Wisconsin, “the contraction of your leg muscles and the pressure of the water helps move blood through the veins”. A 30-minute daily swim workout can achieve multiple benefits for your vein health and your diabets.
- Sleep with pillows under your knees to elevate your feet and lower legs to relieve pressure on your legs.
- Avoid tight waist bands, which put excess pressure on the veins. In addition, elevate your legs above heart level when relaxing.
- Get up frequently while sitting. Do not site for more than 20 minutes at a time. While sitting, do ankle rolles to keep your blood moving. After sitting for 20 minutes, stand up and calf/toe raises to get your blood circulating. March in place for 2 to 3 minutes, and pull your knees up high.
- Consider wearing compression stockings, which may ease pooling of the blood and preserve the already weakened vein. You may need to check on proper fitting of these stockings since they come in various pressures and can be worn on different portions of your legs. Some compression stockings come up to your knees, while others can reach as high as your thighs. Ask your healthcare provider which would work better for you. You should purchase at least two pairs so you can wear one daily and keep one pair freshly washed and ready to go. Replace compression stockings every six months, since the fibers weaken over time from constant stretching and repeated washing. Usually compression stockings are taken off at bedtime, but you may be required to wear them 24 hours a day; check with your physician to see which is best for you.
- Losing that excess weight reduces the detrimental effects of diabetes and varicose veins. Any weight loss will place a lighter load on your entire legs and veins; this reduces unnecessary pressure on your veins.
- Attend all of your doctor’s visits, the extra pair of eyes monitoring your legs and vein health is beneficial.
Products:
Consider using pure essential oils if approved by your doctor. There is “no current concrete research stating essential oils will help varicose veins”. Lavender, ginger, and peppermint oil may ease pain and reduce inflammation along with giving a calming sensation. Rosemary oil may improve circulation. Always dilute these pure essential oils with water (or a carrier oil, like coconut oil). Gently place the diluted essential oil on a wash cloth, or use your hands to gently rub into the area of concern. Never apply oil or any other product on an open wound on your skin.
- Some recent studies have suggested taking a “500mg bioflavonoid supplement daily”. “Anti-oxidants called oligomeric proanthocyanidins did better than a placebo at reducing swelling, aching and pain associated with varicose veins”. Horse chestnut extract may help small varicose veins since it strengthens vein walls due to a compound called aescin. Some clinical trials showed that “horse chestnut may reduce inflammation and leakage”. Again, always check with your physician prior to starting any of these supplements, since they may have a negative effect on the liver or kidneys. Certain supplements may not mix with your current prescription medications.
- Try not to cross your legs and if you must, do so for short periods of time crossing at the ankle only. Site in a chair where both your feed can easily rest on the floor comfortably, or place a box or tray beneath your feed to help support them.
- Eat an adequate amount of fiber. Fruits, vegetables and whole grains promote regularity and regularity eases pressure on all of your veins. Ask your physician if you should take a fiber supplement, such as Metamucil, if you are not achieving bowel regularity from fibrous foods alone. Remember to drink a sufficient amount of water while increasing fiber content.
- Try to reduce sodium content in food which will help reduce leg and vein swelling. Processed foods and refined carbohydrates are not good for diabetes or vein health, because they are high in sodium. Sodium increases water retention, which negatively affects blood circulation.
- Eat foods that have high potassium, this helps decrease water retention. Some high potassium foods include bananas, cantaloupes, oranges, grapefruits, and cooked spinach. Watch your portion sizes if you are counting carbohydrates.
- Avocadoes are excellent for vascular health. They are packed with vitamin C, which forms collagen and elastin, and makes veins more supple. Avocadoes also contain vitamin E which may reduce the chance of blood clots, common with varicose veins.
- Flaxseeds decrease bloating and pressure on your legs. Put them on yogurt or cereal or eat as a snack.
- Rosemary can be used as a dried or fresh spice, sprinkled on chicken, lamb, beef, or potatoes. Rosemary can improve circulation.
- Beets contain betacyanin. Betacyanin may reduce the amount of homocysteine, which leads to inflammation and blood vessel damage. Eat beets as a side dish, put on salads or drink pure beet juice.
- Green tea has up to 200 milligrams of polyphenols. Polyphenols can decrease swelling and strengthen your blood vessel walls. Green tea also has quercetin which reduces inflammation.
- Reduce or eliminate alcohol because it dehydrates you, which makes it more difficult on your circulation system.
Medical Forms of Treatment
There are multiple ways to treat varicose and spider veins performed by board certified vascular surgeons or cardiologists with special training.
- The ambulatory Microphlebectomy procedure is done in the office with local anesthesia. Tiny cuts are made over the veins and they are “teased out with surgical hooks”. There is minimal pain and down time.
- Ultrasound-guided chemical ablation or sclerotherapy works for deeper veins that can’t be treated by a laser. A chemical, such as salt solution or foam, is injected into the vein with guidance from an ultrasound. A pressure bandage is then placed to help seal the vein shut and help the vein be reabsorbed into surrounding tissue. The blood is now diverted to normal functioning veins. There may be some bruising and swelling, but these symptoms are usually mild and disappear quickly.
- Endovenous ablation involves a thin catheter with laser energy being threaded down the vein by the physician and is used to cauterize or burn the damaged vein. The heat from the laser then seals it off. It is usually performed on the great saphenous vein, which can back up and cause a “varicosity” or bulging in smaller veins. Treatment usually takes an hour but recovery can take up to two months. You will need to wear compression stockings and stay off your feet as much as possible in the beginning.
Newer Treatment Options for Varicose Veins
Vascular specialists are suggesting several newer treatments, such as:
- VenaSeal is relatively new (2015) and is just now starting to be covered by health insurance (as of 2018). It permanently treats the problem and seems even easier than laser treatment. This procedure is for patients who have annoying symptoms such as blood clots, open skin ulcers, and pain. VenaSeal is an outpatient procedure. “An adhesive similar to super glue is injected into the vein and seals them off after applying pressure”. The risks of complications are low with this procedure and patients experience minimal down time and bruising.
- MOCA, or mechanochemical ablation, is similar to thermal ablation, but does not use heat. MOCA uses an infusion catheter that “agitates the vein lining with a rotating wire tip and injects a liquid sclerosant (solution agent) to close and seal the vessel.” There is no need for anesthesia and this option poses a low risk of nerve damage.
Although varicose and spider veins are often just a cosmetic problem, many people also suffer with painful symptoms. Your risks for these vein issues increases with diabetes.
Have a question or comment? Post below or email me at [email protected] if you would like to share them with ADW Diabetes.
NOTE: Consult your Doctor first to make sure my recommendations fit your special health needs.

 Consider using pure essential oils if approved by your doctor. There is “no current concrete research stating essential oils will help varicose veins”. Lavender, ginger, and peppermint oil may ease pain and reduce inflammation along with giving a calming sensation. Rosemary oil may improve circulation. Always dilute these pure essential oils with water (or a carrier oil, like coconut oil). Gently place the diluted essential oil on a wash cloth, or use your hands to gently rub into the area of concern. Never apply oil or any other product on an open wound on your skin.
Consider using pure essential oils if approved by your doctor. There is “no current concrete research stating essential oils will help varicose veins”. Lavender, ginger, and peppermint oil may ease pain and reduce inflammation along with giving a calming sensation. Rosemary oil may improve circulation. Always dilute these pure essential oils with water (or a carrier oil, like coconut oil). Gently place the diluted essential oil on a wash cloth, or use your hands to gently rub into the area of concern. Never apply oil or any other product on an open wound on your skin.











Thanks for the details about varicose veins. I will definitely follow your given steps for varicose vein treatment.
Is there any non surgical treatment or therapy for varicose vein treatment? Thanks.