Here are two questions I addressed during our diabetes self management skills program this week. Although they are about different issues, the questions were asked by patients who have diabetes. You may have personally experienced these problems. Please feel free to write to ADW Diabetes if you have other questions you would like answered.
Question 1: “I recently had a pedicure and ended up with an infection that requires treatment at a wound care center. How is this possible?”
I know it is the end of summer, but living in Florida allows patients to have pedicures year round. Although less common, many men go for pedicure services instead of trimming their own nails. This particular patient has required debridement (tissue removal) as well as hyperbaric oxygen treatments for an infection caused from a pedicure. Here are a few recommendations to follow when you choose to have a pedicure – especially when your diabetes is uncontrolled.
- Do not shave your legs, ankles or tops of your feet prior to a pedicure. Wait a few days after shaving to make sure there are no nicks or cuts caused by the razor blade. Use an electric shaver, which will cut down on nicks or skin openings. Make sure if you use a razor blade that it is clean and sharp. Wait to apply lotion after shaving, as this could cause irritation.
- Skip that appointment. Many people have standing appointments and feel they need to keep the appointment, even if they have a cut or open wound. They will understand since you are a regular customer. Do not go with an open wound – see your medical doctor.
- Pick your salon carefully. There are nail salons in every strip mall in the state of Florida. I tell my patients to ask questions. They should ask about sterilization of the tools and equipment. Do they use an autoclave or disinfecting solution? Even better, bring your own tools to be cleaned properly by them with each appointment. It is best when they are bagged and opened when you have your appointment. Make sure the shop owner knows you have diabetes. Change out instruments and tools when they get dull.
- Request separate foot bowls. Before salons had fancy massage chairs with attached whirlpool foot bowls, they used small separate bowls that did not require drains. It was easier to keep them clean without a drain attachment. Some shops use individual disposable liners, which is an added benefit. Make sure they clean with a disinfectant.
- Have a relationship with your technician. It is important for them to know you have diabetes. Try to establish a relationship with one specific person if possible. Watch out for abrasive tools and blades which remove calluses and corns. Ask for pumice stones that are gentler to the skin. If you have rough areas, consider seeing a podiatrist for these problems and go to the salon only for lotion and polish change.
- Nail length. Make sure your nails are trimmed well, but not too short. Have them trimmed straight across with a clipper. Have them use an Emory board to round out the rough edges.
- Watch your cuticles. The rough skin around your nail bed should be soaked and gently pushed back with an orange stick. Do not allow this tissue to be cut since it is protective. Use cuticle oil if your cuticles are especially dry.
- Go for a dry pedicure. These are becoming more popular, since soaking can increase the risk of fungus in your nails. If you choose to soak, do not go overboard. Nail fungus is extremely common in people with diabetes. It is not dangerous, but makes it more difficult to trim the thick and hard nails. If you are unsure – go to your podiatrist. Fungus can be treated with paint on solution or with an oral medication. Liver enzymes should be monitored if you choose to take the oral medication. You should remove nail polish when you have fungus, to allow the nail to breathe and heal. Once the fungus heals, be careful – since you will be at increased risk of future episodes of nail fungus.
Having a pedicure should be a relaxing and pleasurable experience. As long as you follow certain guidelines you should not have a problem. Consult a medical professional if you notice an infection, sore or open wound as soon as possible and do not self treat.
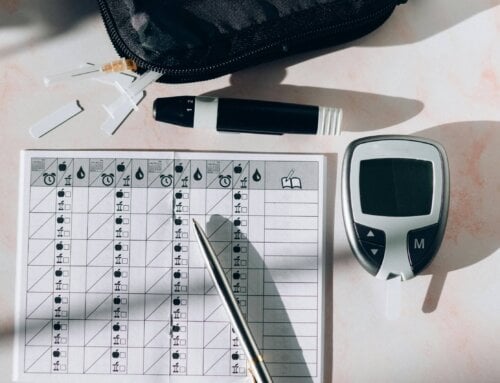
Question 2: “I am new to diabetes and overwhelmed! What are 3 things I can easily do today to help control my diabetes? I promise to get more involved but give me a chance!”
The list could obviously be much longer since diabetes is a 90% self managed and maintained disease. Since he was having difficulty focusing on all the new information, I offered him some quick tips that are easily accomplished. We will address more changes at our next visit.
- Get a complete eye exam from an optometrist or ophthalmologist. Make sure they dilate the retina. The optometrist can perform the entire exam, but does not do surgery. Wear sunglasses at all times when outdoors, since diabetes increases your risk of cataracts, glaucoma and retinopathy. Rest you eyes for 10 minutes when looking at a computer screen for an hour or more. Talk to your physician about moisturizing drops if you suffer from dry eyes. Wear protective glasses when doing home projects.
- See your dentist. A complete mouth exam – including checking for gum pocket depth – is extremely important. Gum (or periodontal) disease is a sign of inflammation and is linked to a higher risk of heart disease. It often causes blood sugar elevations and should be dealt with immediately. If it is too involved for your regular dentist, ask for a recommendation of a periodontist. Floss daily, use a complete toothpaste and brush with an electric toothbrush twice daily. Gargle with a mouth rinse, especially if you suffer from dry mouth. Medications and out of control blood sugars can cause dry mouth, which increases dental and mucosal problems. Make follow up appointments as needed and make routine visits at least twice a year.
- Move! He has never really exercised, and at 68 years old just the thought made him more anxious. I did not recommend a formal exercise program or gym membership, but we did discuss moving out of his easy chair every hour (stand and move). He was willing to do leg lifts in his chair, do additional stretching and walk to the end of his driveway three times a day. As long as I convinced him to move more, he was on his way to decreasing his insulin resistance and controlling his blood sugars!
These are simple but important questions asked by patients like you who need some guidance. Never think your question is silly or unimportant. Each of you probably has many questions that often go unanswered. Be proactive and get the right answers!
NOTE: Consult your Doctor first to make sure my recommendations fit your special health needs.












Hey There. I discovered your blog using msn. This is an extremely smartly written article.
I’ll make sure to bookmark it and return to learn more of your helpful info.
Thank you for the post. I will certainly return.
I have type II diabetes, my A1C is below 6.5 but I am having issues with my feet having a strong burning sensation though they feel normal temperature.
This is especially annoying when I go to bed. The sensation isn’t always there but, especially at bed time, is usually present. I have no foot sores or rashes.
Thanks for your question about neuropathy and diabetes with a controlled A1C. Often people who suffer with diabetes for 10 years or longer, even with controlled numbers suffer from symptoms of neuropathy. You did not mention how long you have had diabetes. You feel the symptoms especially at night since your body slows down and you are lying still. You may not realize that you are having high blood sugar swings even though your A1C is controlled since it is an average. Also neuropathy has many other causes besides diabetes including back issues. You should check with a vascular physician and see if further testing is needed. Stay as active as possible, protect your feet with proper shoes and socks at all times and do not smoke. If you are still suffering from problems ,there are medications that can help with the symptoms. Best of luck! Nurse Robbie
Please, anbody with diabetes should ONLY see a Retina specialist. I am a diabetic of 52 years. I get my eyes examined every 6 months and have not had any problems UNTIL 12-16-2012! I had been seeing a Corneal specialist for the past 10 years. He has performed both of my catarac surgeries. At each exam he would tell his aid about slight bleeding around the periphery of the retina but he never felt it necessary to take a picture of the retina with the injection to highlight any bleeding if there was any. I went blind in my right 2 months after having my last exam!! While he is a wonderful CORNEA SPECIALIST, he is not a RETINA SPECIALIST!!!!! A retinal doctor goes to 2 more years of schooling and is looking more closely at your RETINA than any other Opthamologist. I would never trust my eye exam to an OPTOMITRIST!! They do not have anywhere near the amount of schooling needed to examine a diabetic eye!! This is not a knock on any of the doctors I have mentioned. They just have do not have the specialty training need to keep a closer look on the retina that a diabetic needs. MAYBE, IF YOU HAVE JUST BECOME DIABETIC YOU CAN BUT NOT FOR LONG!!!!
Obviously I am a Type l diabetic and have my own problems to deal with. I have always been a healthy diabetic and losing my vision was the first BAD condition I have suffered. My doctor says that ALL DIABETICS, after 20 years will be sitting in “THAT CHAIR” with eye problems, diabetic related. I am not trying to scare anyone, I am just trying to help others so that maybe they will not suffer the difficulty that I did. After 2 surgeries, I got my vision back and I am working harder than ever to keep myn A1c down to a healthy level. Sorry about this long airing of my problems but I hope it will maybe help other diabetics in their struggles with this illness.