Obesity is one of the biggest health problems in the world with over 90 contributing factors. There is no single solution to prevent obesity. In 2013, it was finally recognized as a true “illness or disease”. Obesity is one of the top risk factors in developing type 2 diabetes. “Diabetes is 93% higher when you have a body mass index (BMI) of over 35 kg/m2“. According to Endocrine Today, a professional journal, “more must be done across the fields of cardiology, endocrinology and obesity medicine to improve the management of patients with diabetes”.
Even after decades of research, diabetes still has no cure and remains one of the most expensive illnesses confronting our health care system. Annually, the diabetes management cost in America is $330 billion. Aside from finances, it takes a huge personal toll on patients and their families. On-going research in the field of obesity and diabetes remains essential. New drugs continue to be developed, clinical trials are being conducted, and more equipment and diagnostics are available. This is good news. Recently, Covid-19 adds another negative dimension, especially if you are obese or have diabetes.
Obesity & COVID-19: What happens if you are obese or have diabetes?
- Both conditions are associated with higher rates of bacterial and viral respiratory infections.
- Obesity and diabetes cause chronic and systemic inflammation.
- Obesity and diabetes both weaken the immune system functions.
- According to CDCs Morbidity and Mortality Weekly Report, April 2020, “90% of hospitalized patients with Covid-19 have a chronic condition. 48% have been obese and 28.3% have had diabetes, so far.”
- Recovery is lengthier with more complications if you are obese or have diabetes.
Have your eating habits changed because of COVID-19?
The short answer is a definite yes!
- Since the start of the outbreak in March 2020, eating habits have changed for the worse: 41% of those 18-35 years, have increased their daily snacking by 26%.
- People with children snack more than people with no children.
- Women snack more than men.
- Snacking choices have been poor due to constant stressors and additional daily pressures.
- Budget constraints due to job furloughs, salary cuts and job firings lead to choosing and eating more junk foods.
- “Food supply scares” are real. In the early part of 2020, some meat processing plants were closed due to COVID-19. Farmers had problems delivering fresh foods. Many are afraid to shop in the market. Trying to boost your immunity with wholesome foods has become more difficult.
- Many people are ordering fast foods such as burgers, fried chicken and pizza since it is cheap, tastes good and can be easily delivered.
- Taste and price have become the number one priority for many of us. Healthy food has slipped away.
- All these latest eating trends will only add to the obesity and diabetes crisis.
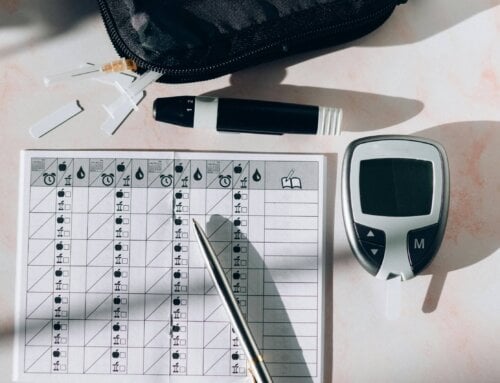
How do you determine obesity?
Obesity is when you carry excess body fat. It involves both the size and amount of fat cells. Defined by the National Institutes of Health (NIH), “Obesity is considered a BMI of 30kg/m2 or above”. Morbid obesity is over 40kg/m2. BMI (body mass index) is “weight in kilograms divided by height in meters squared”. You can easily obtain your BMI using online calculators or smartphone apps. Electronic medical records can automatically calculate your BMI if you enter both height and weight. Muscular people may have an elevated BMI without being obese. BMI categories include:
- Normal weight: 18-24.9
- Overweight: 25-29.9
- Obese: over 30
- Morbid obesity: over 40
Besides a BMI measurement, a health history and general exam should be performed by your health care provider. Bloodwork is also necessary before a diagnosis can be made. Waist circumference measurement has become another easy and standard test. It is effective and low cost but must be performed correctly. A simple tape measure should be placed at the widest point of your abdomen. A measurement of over 35 inches for women and over 40 inches for men signifies excess abdominal or visceral fat. This is considered unhealthy fat distribution and can often be tied to your genes. Abdominal fat can be related to several other chronic health conditions including diabetes.
What are common causes of obesity?
The common denominator in obesity stems from an energy imbalance. Basically, there are too many calories going in and not enough energy expenditure going out. Obesity is so much more than just overeating, choosing poor foods and lack of movement. It is a combination of behavioral, genetic, medical, educational, ethnic, and financial factors.
Biological Factors
- Genetics. If your parents/siblings are obese, your risk goes up due to genetics. If you were an obese child, your risk goes up to be an obese adult. Everyone has a different metabolic rate, and this rate can be manipulated. Some people start with a higher metabolic rate and burn more calories just because of their genes. Your genes can also affect your hormones. “Leptin deficiency” is common among family members. Leptin is a hormone which helps regulate your weight by signaling the brain when body stores of fat are too high. You tend to stop eating when you are full. Replacing leptin is currently under investigation. Family members tend to develop similar eating and exercise habits which is partially blamed on genetics.
- Aging. The older we get the more muscle mass we lose and our metabolism decreases. This allows for weight gain and more of a chance to develop obesity.
- Ethnicity. Minorities tend to be more obese. Historically, African Americans and other Blacks have the highest rates of obesity, with Hispanics not far behind. Some causes are lower levels of income, less access to healthcare, education, social conditions, and personal eating preferences developed within the family.
- Your microbiome. More and more research points to your gut bacteria diversity and the chance of obesity. The known factors are: highly processed, packaged foods and sugar lead to less gut diversity and eating wholesome fresh foods enhances gut microbiome diversity. The more diverse your gut microbiome, the less chance of obesity.
External Factors
- Aggressive marketing. Over-zealous commercials, tag lines, food placement on shelves, fancy store displays, advertising labels, buzz words, marketing directed at children, and ornate and colorful packaging can all contribute to the obesity crisis.
- Medications. Included are anti-depressants, certain diabetes medicines such as insulin and sulfonylureas, antihistamines for allergy sufferers, blood pressure medications and beta blockers, anti-seizure medicines and steroids including Prednisone. Steroids encourage weight gain since they cause you to retain excess fluid and develop a large appetite.
- Modern day living. Using cars, electric bikes, people movers in airports or train stations, elevators, escalators, remote controls and computers has helped pave the way for obesity.
- The word obesogen was coined in 2006. They are chemicals that are toxic to humans and animals and interfere with hormonal function. Also known as, “endocrine disruptors” they cause weight gain and are presently contributing to the obesity crisis. They increase the sensitivity of gaining weight especially when introduced during development and at a young age. Obesogens can change how you regulate feelings of hunger and fullness, how fat cells develop and the number of fat cells that are made. Common obesogens are cigarette smoke, air pollution and flame retardants used on furniture, rugs and clothing. PCBS used in paints, adhesives and sealants, as well as BPAs used in plastics and to line canned foods. Parabens found in cosmetics, air fresheners and scented wax candles can also pose a problem.
Internal Factors
- Sleep changes. Lack of sleep and sleep quality can put the pounds on due to chemical changes. Less sleep or interrupted sleep allows for more snacking time and over-indulgence.
- Western diet. High fat intake, high sugar intake, fast foods, huge portion sizes, constantly snacking, and processed foods can lead to obesity.
- Mental health. Stress, anxiety, anger, boredom, frustration, sadness, and isolation are all mental conditions that are relevant at this time. These “states of mind” can trigger binge eating, excess snacking and mindless eating.
- Lack of exercise. Hours spent in front of a screen, sheer uninterest, physical limitations, lack of a safe place to walk, no gyms or classes due to coronavirus.
- Simple excessive carbohydrates. Sodas, energy drinks, fruit drinks and juices, cocktail mixers, too much beer, wine, alcohol, desserts, snacks and refined foods. Simple carbohydrates quickly turn to sugar, increase insulin release, add to your insulin resistance, and weight gain.
- Smoking cessation. As wonderful and necessary as smoking cessation is, it can certainly lead to overeating and obesity by substituting one addiction for another.
Can obesity trigger other problems?
Obesity is way more than just a cosmetic concern, and is associated with an array of serious medical conditions. Obesity can increase your risk of certain cancers such as breast, ovarian, prostate, endometrial, colon, rectal, kidney, pancreatic, and esophageal. Your risk of heart disease increases along with more heart attacks, heart failure, hypertension and high cholesterol levels. Risk for developing diabetes goes way up with insulin resistance, metabolic syndrome and non-alcoholic fatty liver disease (NAFLD). Sleep apnea, gall stones, gout, GERD or gastric reflux, urinary incontinence and lung issues including shortness of breath, are more common with obesity. Arthritis and orthopedic issues including knee and hip replacements occur more frequently. Emotional problems are higher with obesity. Finally, there are many sexual dysfunction issues related to obesity including low testosterone levels, erectile dysfunction, infertility issues and menstrual problems.
Current obesity rates in the United States
According to the CDC in 2018, “42.4% of Americans were obese”. In 2020, 2/3 of Americans are overweight and one in three Americans are obese. The rates continue to grow. Middle age Americans have the highest rates of obesity. In the US, 49.6% of Blacks, 44.8% of Hispanics, 42.8% of Whites and 17.4% of Asians are currently obese. Obesity can cause social isolation, decreased work achievement and shame or guilt. It can influence the doctor/patient relationship by causing lack of trust and “head-butting”. Many health practitioners have limited expertise with obese patients. They do not supply oversized blood pressure cuffs, scales, exam tables, gowns or office chairs. Doctors are not trained in altering medication doses for the obese who may need more. There is no medical school training specifically geared to teach students about obesity.
How easy is it to lose weight?
Treating obesity is not easy and losing weight is one of the most difficult things you can ever do. Even after losing weight, most people regain it within 5 years. Work with your health care provider on achieving a “healthy weight”, and not a perfect weight. Everyone has a different healthy weight based on a multitude of factors.
Obesity: is there any good news?
The good news is that even modest weight loss of 5-10% of your total weight can lead to health improvements and a reduction in disease progress. Blood sugar, blood pressure and cholesterol numbers will go down with weight loss. Orthopedic problems may resolve with weight loss.
What can you do to help avoid obesity?
- Get a team in place. Usually it takes a physician, dietitian, and a mental health counselor to help you achieve and maintain weight loss. Keep your family and friends involved!
- Join support groups. There are specific resources at Over-eater’s Anonymous, Weight Watcher’s, Obesity Society and The Obesity Action Coalition. Your hospital or physician may recommend another local group.
- Move more. Use personal trainers, online classes, videos, home equipment, swimming pools. Just walk. Do resistance training with bands and weights. Lifting burns calories. Move arms and legs while sitting in the chair. Participate on a team sport. Anything you can commit to is worthwhile.
- Apps. There is scientific evidence supporting these apps and weight loss. Some popular ones include: My Fitness Pal, Noom, Lose It, FitBit, Fooducate and Body Weight planner.
- Pedometer. Even an old-fashioned pedometer will make you aware of how many steps you take.
- Know and avoid food traps. What triggers your out of control eating behavior? Avoid those triggers. Write in a journal. Look for patterns. Do not miss meals. Avoid drastic, unrealistic or the “latest fad diet plan”. Make sure you are not missing nutrients. Ask about vitamins and supplements.
- Monitor weight regularly to at least weekly to keep you on track. Understand everyone’s weight can fluctuate daily.
- Eat more foods high in fiber. Eat lean protein. Avoid heavy sauces, creamy dressings and food additives.
- Drink only calorie-free beverages.
- Consider weight loss medications under the supervision of your health care provider.
- Weight loss surgery may be a viable option depending on your BMI. Your team as a whole should make this decision. Remember, the bariatric surgery can help you lose weight, but your behavior must permanently change to keep the weight off.
More than ever, during stressful times, you may have a temporary breakdown in maintaining your weight. The priority should be having a good nutritional plan and maintaining your overall health. Know you can stay healthy with knowledge and a solid plan in place.












Leave A Comment